Thoracic outlet syndrome definition.
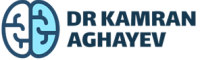
The thoracic outlet syndrome, or simply TOS, is a general term describing several conditions associated with compression of nerves and/or blood vessels in the thoracic outlet area, which represents the upper exit (outlet) of the chest cavity.
What is the thoracic outlet area?
The thoracic outlet is a heart shaped area located at the top of the chest cavity. Structurally, this area is bounded by the first thoracic vertebra, the left and right first ribs, and the sternum. It contains important organs and therefore has great clinical significance.
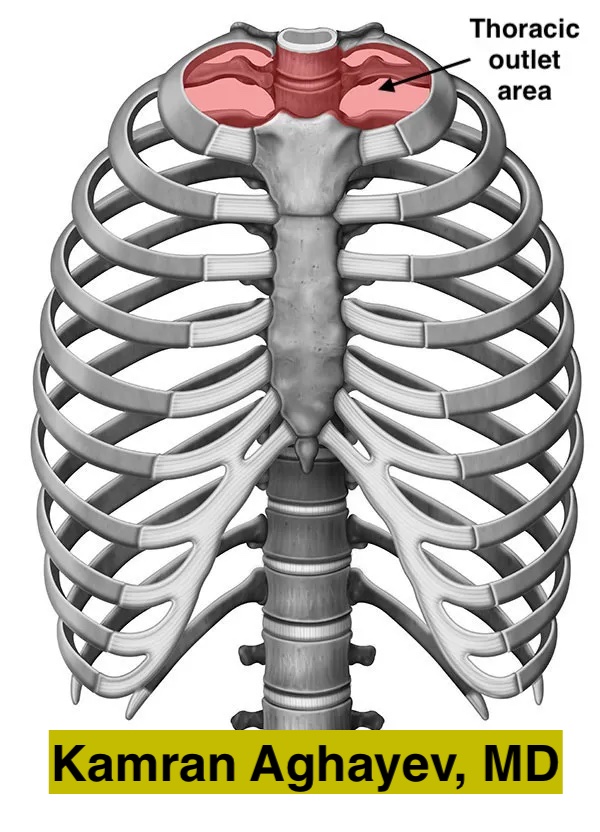
What structures are affected by TOS?
The neuro-vascular bundle is pressed in thoracic outlet syndrome. In summary, this bundle includes the brachial plexus, the subclavian artery and vein.
Brachial plexus
Five nerves coming off from the spinal cord (C5, C6, C7, C8, and T1) form a complex network called brachial plexus. Consequently, the brachial plexus branches off several nerves that travel to neck, shoulder, upper chest and the arm. Basically, these nerves carry impulses between the spinal cord and the arm. They control every aspect of arm and shoulder function: skin sensation, muscle movements, sweating, blood vessel tone, etc.
Subclavian vessels
The subclavian artery and vein are main vessels providing blood flow to and from the arm. They pass above the first rib alongside of brachial plexus on their route to arm.
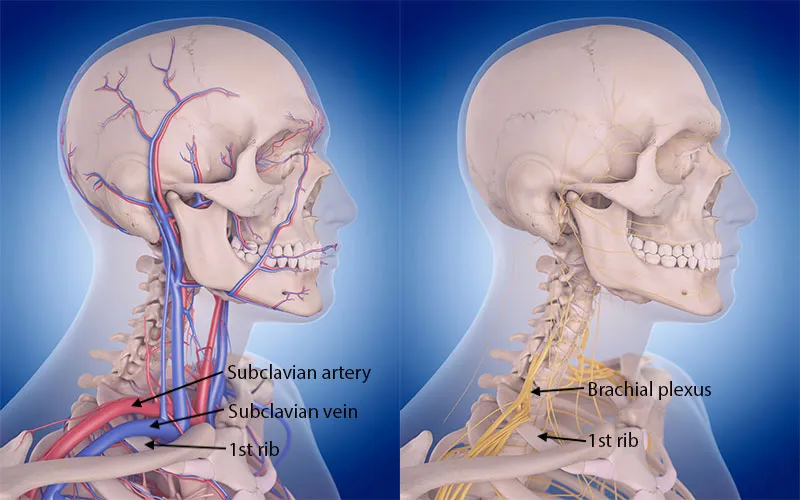
Anatomical relationships in thoracic outlet area
The nerves and vessels travel directly above the first rib which has two specific grooves to fit subclavian artery and vein. Additionally, C8, T1 nerves roots and lower trunk of the brachial plexus also directly touch the first rib. The brachial plexus and subclavian artery pass through a narrow anatomical window called the scalene triangle. This triangle has three borders – two scalene muscles (anterior and middle) and the first rib. The subclavian vein on the other hand passes through costoclavicular or venous triangle. Subclavius muscle, anterior scalene musce and the first rib form venous triangle. Subclavius muscle may smash the vein against the first rib.
Thoracic outlet syndrome forms
There are three clinical TOS forms:
- Neurogenic TOS – nTOS. The most common form – approximately 80-85% of cases. Compression affects the brachial plexus and symptoms develop due to neural compression.
- Venous TOS – vTOS. Far less common – about 10-15% of cases. Compression affects the subclavian vein and symptoms develop due to insufficient blood return from the arm.
- Arterial TOS – aTOS. The least common form – approximately 1-2% of all cases. Compression affects the subclavian artery and the symptoms develop due to insufficient flow to the affected arm.
Causes of thoracic outlet syndrome
The thoracic outlet syndrome is a term describing the site (location) of disease rather than the cause. This term is similar to other entrapment neuropathies, for example carpal tunnel syndrome. Generally, it is customary in peripheral nerve surgery to classify the conditions according to pathology site. However, the term doesn’t contain information about the cause of the problem. Occasionally, the compressing factor can be obvious (like cervical accessory rib or a tumor) on imaging studies. Unfortunately, this is not the case for the majority of patients even with advanced imaging.
There are several conditions predisposing to thoracic outlet syndrome. Women are affected 3-4 more often than men. Sometimes, people working with repetitive arm and hand movements develop TOS. Bad body posture, particularly shoulder slouching can cause compression. Various congenital and acquired conditions responsible for TOS development are summarized below:
Cervical accessory rib
There are 12 pairs of ribs in normal human body which form chest cavity. Occasionally, people may have accessory or extra cervical ribs. Recently, a large literature review has found that approximately 1.1% of population has cervical ribs.1. Furthermore, the occurrence of accessory cervical ribs in TOS patients is 29% – approximately 25 times more than in general population.1.
The shape and size of the rib may vary dramatically – from a slightly longer C7 transverse process to almost normally looking rib. If extra rib is big, its tip usually touches the first rib. X-ray explicitly shows cervical additional ribs, yet unexperienced eye may fail to recognize them.

Genetic causes of anomalous cervical ribs
Unfortunately, the exact mechanism responsible for additional cervical rib formation in unknown but there is evidence that it might be due to glitch in HOX genes. HOX genes or homeobox genes are responsible for sequence of events responsible for correct body segmentation. Disturbances and mutations affecting these genes lead to number of vertebral anomalies and cervical ribs. Studies showed that mice with mutant HOX genes develop additional ribs at seventh cervical vertebra.2. Interestingly, HOX genes also play certain role in cancer development and there is evidence that the occurrence of additional ribs is higher in cancer patients further supporting HOX hypothesis.3.
First rib abnormalities
First rib is a curved flat bone lying between the first thoracic vertebra and sternum. Anomalous, broken or misplaced first ribs can cause TOS by stretching or compressing the neuro-vascular bundle. Congenital abnormalities such as fused ribs or bifid ribs are well-known causes of TOS. One study found that thick first ribs may cause TOS.4. Another study found that abnormal bone prominence near the sternal end of the first rib is responsible for venous TOS development.5.
Trauma is also a significant contributor to TOS. Fractured first ribs may not heal appropriately. As a result, fracture site may develop either excessive bone callus formation or pseudoarthrosis (lack of bone healing leading to tumor like swelling). These inappropriately healed first ribs can also cause thoracic outlet syndrome. Tumors of the first rib including benign lesions like hemangiomas expand the bone and compress nearby neuro-vascular bundle.
Like in case of cervical ribs plain X-rays can diagnose first rib abnormalities. However, complex anatomy of the first rib, overlapping nearby bones and variety of first rib pathologies make diagnosis difficult for an untrained eye. Therefore, only experts with vast experience can correctly pinpoint first rib abnormalities on X-rays. CT scan with 3D reconstruction can visualize first ribs much better than X-rays and is a superb imaging modality when it comes to bone abnormalities.
Fibromuscular soft tissue bands
Fibromuscular soft tissue bands constitute significant portion of TOS cases. Occasionally, the cause of compression may be an abnormal muscle, a fibrous band, or a combination of them. For example, abnormal muscle lıke scalenus anticus, scalenus minimus and subclavius posticus can cause neuro-vacsular compression yet they are relatively rare. These bands of fibro-muscular tissue run from various portions of the spine (usually from C7 transverse process) to the first rib stretching and compressing the neuro-vascular bundle.6.
Hypertrophic muscles
Hypertrophic muscles also may cause neuro-vascular compression. People extensively using their arms and hands for work and sports are especially prone to this type of TOS. Naturally, athletes frequently develop TOS. Scalene muscle hypertrophy usually results in n- and a-TOS (since both the artery and brachial plexus run inside the scalene triangle).7. Sublclavius muscle hypertrophy on the other hand may cause compression and even thrombosis of the subclavian vein (Paget–Schroetter disease).
Costo-clavicular compression
Both clavicle and first rib make joint with upper part of sternum. First rib has little mobility whereas clavicle is a very mobile bone. Clavicle makes another joint with the scapula. It is basically is a lever between fixed sternum and mobile scapula. Normally the gap between the clavicle bone and the first rib – costo-clavicular space is quite wide. Neuro-vascular bundle passes through this gap just above the first rib and below the clavicle. However, with arm abduction costo-clavicular gap may become very narrow due movement of the scapula. This effect is called “nutcracker mechanism” and may narrow costo-clavicular space. Studies show that in normal people the gap remains wide enough so there is no pressure on nerves and vessels. In TOS patients the gap may become critically narrow and result in neuro-vascular compression.8.

Blood vessels
Occasionally, blood vessels branching from subclavian vessels may loop around the brachial plexus and cause compression. These small vessels causes are very difficult to diagnose radiologically and usually discovered during surgery.9.
Chronic kidney disease and dialysis
Arterio-venous fistula provides easy vascular access in hemodialysis patients. However, major problem is an increased blood flow and turbulence in the subclavian vein. This leads to central venous narrowing and the thoracic outlet area is a particularly vulnerable region. Like in most vTOS cases, such stenosis usually develops in the costo-clavicular (or venous) triangle due to “nutcracker effect” between the clavicle and the first rib.10.
Next: Thoracic Outlet Syndrome Signs and Symptoms
References
- Henry BM, Vikse J, Sanna B, et al. Cervical Rib Prevalence and its Association with Thoracic Outlet Syndrome: A Meta-Analysis of 141 Studies with Surgical Considerations. World Neurosurg. 2018;110:e965-e978. https://doi.org/10.1016/j.wneu.2017.11.148 [↩] [↩]
- Horan GS, Wu K, Wolgemuth DJ, Behringer RR. Homeotic transformation of cervical vertebrae in Hoxa-4 mutant mice. Proc Natl Acad Sci U S A. 1994;91(26):12644-12648. https://doi.org/10.1073/pnas.91.26.12644 [↩]
- Merks JH, Smets AM, Van Rijn RR, et al. Prevalence of rib anomalies in normal Caucasian children and childhood cancer patients. Eur J Med Genet. 2005;48(2):113-129. https://doi.org/10.1016/j.ejmg.2005.01.029 [↩]
- Chang CS, Chuang DC, Chin SC, Chang CJ. An investigation of the relationship between thoracic outlet syndrome and the dimensions of the first rib and clavicle. J Plast Reconstr Aesthet Surg. 2011;64(8):1000-1006 https://doi.org/10.1016/j.bjps.2011.03.017 [↩]
- Gharagozloo F, Meyer M, Tempesta B, Strother E, Margolis M, Neville R. Proposed pathogenesis of Paget-Schroetter disease: impingement of the subclavian vein by a congenitally malformed bony tubercle on the first rib. J Clin Pathol. 2012;65(3):262-266 http://dx.doi.org/10.1136/jclinpath-2011-200479 [↩]
- Roos DB. Congenital anomalies associated with thoracic outlet syndrome. Anatomy, symptoms, diagnosis, and treatment. Am J Surg. 1976;132(6):771-778. https://doi.org/10.1016/0002-9610(76)90456-6 [↩]
- Qaja E, Honari S, Rhee R. Arterial thoracic outlet syndrome secondary to hypertrophy of the anterior scalene muscle. J Surg Case Rep. 2017;2017(8):rjx158. https://doi.org/10.1093/jscr/rjx158 [↩]
- Illig KA, Doyle AJ. A comprehensive review of Paget-Schroetter syndrome. J Vasc Surg. 2010;51(6):1538-1547. https://doi.org/10.1016/j.jvs.2009.12.022 [↩]
- Hanna A, Bodden LO, Siebiger GRL. Neurogenic Thoracic Outlet Syndrome Caused by Vascular Compression of the Brachial Plexus: A Report of Two Cases. J Brachial Plex Peripher Nerve Inj. 2018;13(1):e1-e3. https://doi.org/10.1055/s-0037-1607977 [↩]
- Davies MG, Hart JP. Venous thoracic outlet syndrome and hemodialysis. Front Surg. 2023;10:1149644. https://doi.org/10.3389/fsurg.2023.1149644 [↩]